10 years ago more than half of San Diegans could see a doctor within two days, today that number has fallen to just 20% of San Diegans, or 1 out of 5
By Amber Frias
Wait times to get a doctor’s appointment continue to increase not just in San Diego, but across the country.
It’s a problem we are hearing about more and more.
“I started seeing blood in my urine,” said Robert Browne, a San Diego resident. “I tried to stay calm for a couple of days until I Googled it. And then I realized it could be serious. Super serious, possibly prostate cancer,” Browne said.
“I couldn’t get an appointment, I was told that it would be like a month, month and a half, you know, sometimes two months out,” Browne added.
“I had surgery in July last year and something went wrong and they put a screw there,” said Jesus Magana, a San Diego resident.
“A screw came loose, I went to the same doctor again and he told me to go to another doctor. So I went to another doctor and I have to wait months and months before I can have the surgery with this other doctor,” Magana added.
NBC 7 met both Browne and Magana at a shopping center in Oceanside after making a visit to a local medical center. They both expressed their frustration and confusion about this recent trend.
And they’re not the only ones.
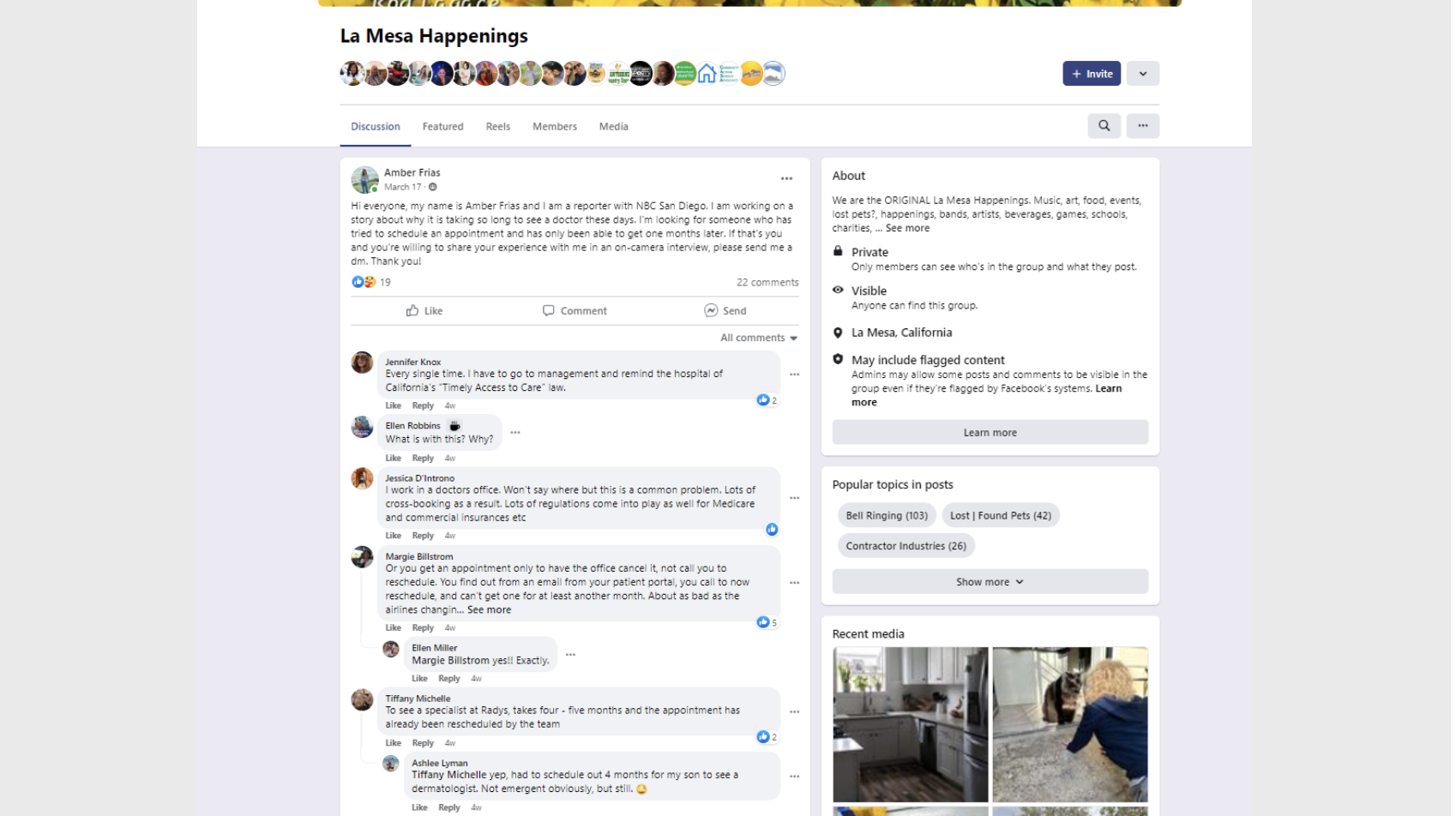
While researching, we posted to a few community pages on Facebook to get a sense of who’s facing this problem. The response was overwhelming. More than 200 people responded to the posts.
Julie Stavros is one of those respondents.
“I’ve been having some issues with my left ear; I feel like something is actually in it,” said Stavros. “I waited a month and a half to see the audiologist. Finally, I got to see them and I found out that I need to get hearing aids. And I cannot get in to be fitted or find out about the hearing aids until the end of June.”
Long wait times are a relatively new trend. In fact, the California Health Care Foundation says 10 years ago more than half of San Diegans could see a doctor within two days, today that number has fallen to just 20% or 1 out of 5.
“We definitely see this on an everyday basis,” said Paul Schalch Lepe, MD.
Lepe is a doctor that specializes in conditions with the ear, nose, and throat.
“Our group is big, and we’re spread out throughout the county, and even with that in mind, oftentimes, the wait times can be upwards of four to six weeks,” said Lepe.
Why the Long Wait Times?
So why the long wait?
“The short answer is we just simply do not have enough clinicians to provide the care that we need here in California,” said Kristof Stremikis, director of market analyisis and insight at the California Health Care Foundation.
Stremikis analyzes data about the state’s care system. He says timely access to medical care is becoming a serious public health threat in San Diego and across California.
“We don’t have the right types of providers in the right places to meet the demand for medical care,” said Stremikis. “Those were problems that predated the COVID pandemic but they certainly got worse because of COVID. But they’re here and they need to be addressed if we’re really going to help people get in and see or get medical care when they need it.”
According to a White Paper by Definitive Health Care, more than 330,000 healthcare providers left the workforce in 2021 alone, with physicians representing the majority.
Burnout
The biggest reason is burnout, according to those we spoke to.
“Doctor burnout, of course, tends to occur when you are overworked, stressed out,” said Lepe. “You have to have many patients to your schedule, sometimes double book, triple book. This makes for long days and patients, of course, are frustrated because they’ve already been waiting very long for their appointments and then perhaps you’re running late in the clinic and it’s this ripple effect.”
According to a recent survey from InCrowd, a healthcare data provider, 30% of physicians said they felt burned out, and about just as many said they would consider leaving the profession.
“I have had the opportunity to mentor and talk down several of my friends from just flat-out quitting medicine,” said Tina Edwards, MD. “They don’t want to do it anymore.”
Edwards from World of Wellness in Oceanside left traditional primary care to start her own practice that does not take insurance.
“A lot of what drove us away from primary care in the first place was we didn’t want to have to see 30 patients a day,” said Edwards. “We didn’t want to have to try to cram a patient into 12-and-a-half minutes. Imagine trying to do that with a patient who’s genuinely ill.”
While Edwards was able to increase the time she spends with her patients, the problem for doctors doesn’t stop at burnout. Many of them are having to spend more and more time dealing with insurance companies.
Insurance Companies
“Now insurance companies, of course, have made their rules for approving procedures or diagnostic tests or any other kind of intervention more and more difficult and more stringent,” said Lepe. “So oftentimes you’ll finally get your appointment, you’ll formulate a plan, perhaps for surgery, perhaps for some advanced testing, and then the test or the procedure gets denied by the insurance for whatever reason. That, of course, leads to an appeal or peer-to-peer communication that is labor intensive. It often leads to very uncomfortable discussions and problems of that nature.”
Making matters worse, according to the Association of American Medical Colleges, by 2034 the number of Americans over 65 will grow by more than 42%.
So we need more doctors to help, right?
Residency Programs and Policy Change
Yes, but there is a problem there as well. Thousands of medical school graduates who are ready to provide care do not get the chance to.
“We have 8,000 medical school graduates every year who cannot become licensed physicians because they cannot get into a residency program because we don’t have enough,” said Edwards.
One of those upcoming graduates is Jason Gomez.
“Unlike other professions like law school, where you take the bar and you’re automatically a lawyer or even in business where you can drop out of college or get an MBA to start a business or to change career path, in medicine, you still have your licensing exam step one, two and three, but you also have to do this residency program,” said Gomez.
Gomez is a medical student at Stanford. He recently wrote about his experience applying for a residency program for the San Francisco Chronicle. In his research, he found that last year, 47,675 medical school graduates registered for “the match,” an online system that pairs new doctors with hospital training systems but there were just 36,277 spots available. That means over 11,000 graduates cannot practice.
“You know, these people are ready to be a doctor,” said Gomez. “They’re at their peak. They’ve finished their clinical rotations. They’ve done their first two board exams. But they’re stuck in limbo in the sense that they can’t actually practice or see patients and so they have to wait a year and some people end up deferring graduation. It’s keeping young doctors from being trained and us as patients from having access to those doctors.”
Stremikis acknowledges the problem but says increasing residency spots requires policy changes.
“We need to increase the overall number, and I’m talking about all types of clinical folks; nurses, RNs, advanced practice nurses, MDs, and community health workers,” Gomez said.
“Really up and down the line, we need more healthcare workers. And we need to make sure we’re utilizing those people in the best way possible,” he added.
The solution won’t come easy and will take time but it’s something Stremikis believes we can’t ignore any longer.
“I think it’s, it’s important for all of us to care and be invested in the solution,” said Stremikis.
According to the Peterson Center on Health Care, the U.S. spends more per capita on health care than any other developed country in the world but has subpar health outcomes. The average life expectancy in the U.S. is lower than in other wealthy nations and about 60% of U.S. adults have a chronic disease.